There is one word in the kidney diet that all CKD patients know—protein. Yet, this protein in the kidney diet remains the source of confusion for most kidney disease patients.
Because they know no better, many physicians restrict the protein intake of their CKD patients early in the disease. Doing this, the physicians only try to apply something universally that should be, in reality, tailored individually. Of course, this practice is not without its harms and could be improved.
I will explain why and how, but let me first lay down some basic concepts that connect dietary proteins and kidney disease.
Is There Much Research?
The topic of low-protein diets and their effect on kidney function came to the fore in the last decade of the twentieth century when the first extensive study showed some benefits of a low-protein diet in kidney disease patients. Since then, the outcomes of such research have been consistent, suggesting the usefulness of a low-protein diet, mostly in slowing down the loss of kidney function.
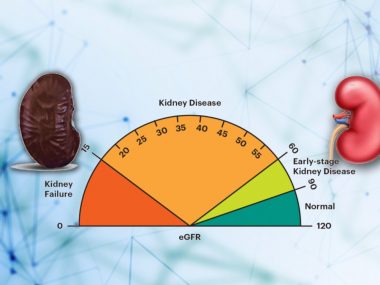
However, most protein intake studies are done on patients with advanced kidney disease, stage 4 or 5, with eGFR 30 or below.
Research has studied both kidney disease populations, diabetics and non-diabetics. However, the benefits are less evident in diabetics than in non-diabetics.
Data on this subject are only sketchy at best, and most guidelines have to extrapolate, or should we say generalize, specific results for all CKD patients.
Protein and Kidneys—A Complex Relationship
The relationship between proteins and kidney disease is quite complex. As a kidney disease patient, imagine a washing machine designed for washing a bucket load of clothes at one time, and you shove two or even three buckets instead. What outcome do you expect? Naturally, the machine may handle the extra burden for a while, but finally, it would break down. High protein in our diet is just like extra buckets of clothes for your blood-washing plant—your kidney.
A high protein diet increases pressure inside the kidney’s filtration units called the glomerulus, leading ultimately to the injury and scarring of the kidney tissue.
Furthermore, a high-protein diet is not just directly harmful to the kidney. As a primary source of nitrogenous waste products, proteins increase the production and retention of acids in the body as the kidney advance toward its later stages. Further still, proteins proliferate the problem of CKD-related bone loss and phosphorus retention—two nagging issues of the late stages of kidney disease.
Protein Diet in Diabetics With CKD
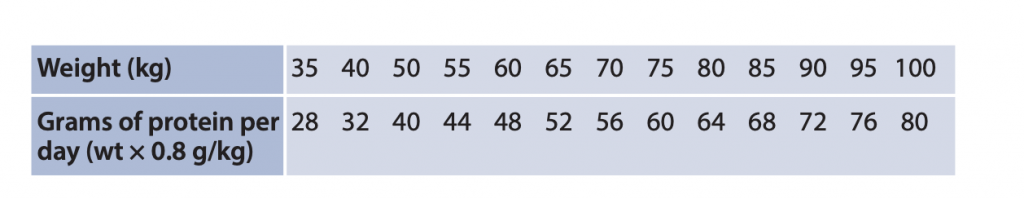
The most recent guidelines recommend 0.8 gm of protein per kilogram of body weight per day for those with chronic kidney disease who are not on dialysis.
For a 70-kilogram adult:
0.8 gm x 70 kg = 56 gm protein per day
Surprisingly, this is the same amount of protein that the WHO (World Health Organization) recommends for a healthy diet in adults. And there are reasons behind this recommendation.
First, the workgroup found only a handful of studies examining the connection between a low-protein diet and kidney disease in diabetics. Despite the high burden of diabetes and kidney disease, they could pull only about a thousand fitting research papers on the subject. The analysis of these papers would yield an even more dismal comment: ” [the group] found no relevant studies, no long-term studies, and inconclusive evidence.
Then diabetes in itself is a complex condition. To regulate blood sugar, people with diabetes restrict carbohydrates, fats, and alcohol. Additionally, these patients often have other co-morbid conditions, such as gout, high blood pressure, and heart disease, which may demand more restrictions, further complicating the dietary regimen.
Restricting protein from an already limited diet, the experts argued, could push these patients over the edge, affecting their quality of life and possibly resulting in malnutrition and weight loss.
Protein Diet in Non-Diabetics with CKD
Protein Diet in Non-Diabetics with CKD
Mainstream guidelines recommend a protein intake of 0.8 gm per kilogram of body weight daily, the same amount recommended for diabetic kidney disease patients.
National kidney foundation, however, recommends lower amounts—0.6 gm per kilogram of body weight daily—for patients with stages 4 and 5.
For a 70-kilogram adult:
0.6 gm x 70 kg = 42 gm protein per day
All the research indicating that low protein intake (compared to normal protein intake of 0.8mg/kg/day) slows down the decline in kidney function studied non-diabetic patients in the advanced stages of kidney disease. In other words, this is the only group where protein restriction showed some benefit.
Is a Very Low Protein Diet Ever Worth It? Rarely

Despite this positive outcome of eating less protein, I hesitate to prescribe low-protein diets to my patients, and for good reasons. First, the severe protein restriction of 0.6 gm per kilogram brings down a patient’s daily protein intake to 42 gm, an unacceptably low amount for an average human, most of whom are used to enjoying about 70 to 100 gm of protein daily. Secondly, as I have discussed in the previous blogs, most CKD patients carry a very low risk of worsening kidney function. Therefore, we need to consider the enormous effort a patient must put in to cut down his protein intake and the cost of supplements that such severe protein restriction mandates. Such restriction is not justified for a vast majority of patients.
Yet, there are a few exceptions. For example, CKD patients with high urine protein ( 2+ or more 300 mg/gm on spot urine test) and patients with rapidly declining kidney function (more than 5ml/min fall of eGFR per year) should consider a very low protein diet of 0.6gm/kg. However, such severe restrictions should always be under the supervision of a nephrologist and a nutritionist.
Protein Diet in Dialysis Patients
The recommended protein intake for dialysis patients is 1 – 1.2 grams per kilogram of body weight daily. For a 70 kg patient, this amounts to 70 to 84 grams of protein daily.
In the body of a dialysis patient, the regular wear and tear are more than in the non-dialysis patient, requiring more protein to maintain body muscles. Furthermore, uremia, the hallmark of dialysis, suppresses appetite, increases metabolism, and malnutrition. So naturally, a dialysis patient needs more than an average amount of protein to keep up with the losses.
Misconceptions
Below are a few misconceptions that need to be addressed, for they can lead to gross calculation errors for dietary proteins.
To calculate protein intake, you need to use the ideal body weight, not the actual weight. For example, if a patient weighs 150 kilograms, he needs to figure out his ideal body weight based on height. This number may turn out to be 70 kg. Now see the enormous error one could have made by using the actual body weight. 0.8mg x 150 = 120 gm of protein per day—a harmful amount for any human being, let alone a kidney disease patient.

Next, many patients wrongly assume that thirty grams of meat equal thirty grams of protein. The quantity of actual protein in any food is less than its net weight. For instance, eight grams of poultry or fish contains only 8 grams of proteins. So, count your protein right and enjoy that extra meat you missed in the meals.