Imagine you suddenly realize that you have a deadline to meet soon. Would you panic or procrastinate? Perhaps, none of the two. You would rather pull yourself together and get down to the task.
For a kidney disease patient, the deadline is dialysis and entry into stage 4 kidney disease, its realization. It is time to do some serious thinking.
While a vast majority of CKD patients never get to the point of end-stage renal disease, a few must prepare themselves for this end, for they would need, sooner or later, some mean to replace their kidney function. The techniques used to replace the role of native kidneys are collectively called renal replacement therapy. There are only three basic techniques for renal replacement therapy: kidney transplant, peritoneal dialysis, and hemodialysis. (Unless you happen to be in India and Pakistan, where magic still works and weird, wild ideas for kidney replacement therapy are still in fashion)
Transitioning to renal replacement therapy is fraught with challenges, and many patients find the details and doings overwhelming despite their regular follow-ups with a nephrologist. As for those, who discover about their end-stage kidney disease suddenly, without having the time to comprehend the situation, they seldom recover from this shock. Therefore, CKD patients had better prepare themselves for this transition by understanding the dynamics of advanced kidney disease, learning about various replacement modalities, and making up their minds before the final moment.
Transition Starts with Discussion
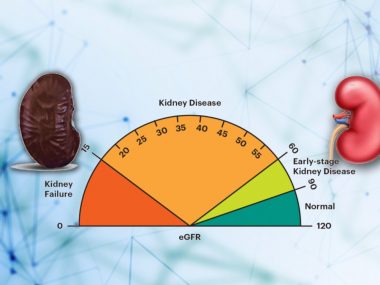
In developed countries, where the healthcare system is not overwhelmed by patients, their poverty, and, above all, their ignorance, where a kidney disease patient starts following up regularly with his nephrologist right from the early stages of the disease, the discussion of renal replacement therapy begins as soon as patient hits stage 4 CKD, that is with eGFR of 30.
The education starts with a simple conversation between a kidney doctor and the patient, the focus of the whole visit being on opening the patient’s mind to the fact that he may need dialysis in the near future, and that it is always better to meet the change well prepared than being surprised.
Next comes the Kidney Smart Class, a no-cost kidney education class, available both online and in person, where a patient learns tips and tools as well as a comprehensive overview of kidney disease. The most important aspect of such educational activities, however, is to know about major dietary changes necessary in advanced CKD, kidney disease complications, and options for renal replacement therapy. What options are out there for renal replacement therapy?
Of note, a kidney disease patient doesn’t have to wait until stage 4 to join the Kidney Smart Class; they are always available, but only a few patients care to educate themselves about their illness unless they face the inevitable.
Kidney Transplant
A kidney transplant is considered the best form of renal replacement therapy. And the best transplant comes from a living donor, whether a relative or a non-related person. Suppose you are eligible for a kidney transplant—a criteria that vary from country to country and depends on your eGFR, age, and other medical conditions—and you have a living donor who wishes to donate you the gift of a kidney. In that case, the next step is the match. The match involves crosschecking the blood and tissue types of the recipient (the patient) and the donor. If the match turns out to be a success, the patient is ready for the transplant surgery. We call this kind of transplant “pre-emptive transplant,” which means getting a transplant without ever needing dialysis.

More often, however, the patients get a cadaveric kidney—from someone who died but had donated his or her organ. For a cadaveric transplant, a patient is placed on the transplant list, usually when his eGFR hits 20. After being listed, a patient may have to wait several years before a cadaveric kidney is available. Remember that the system of cadaveric kidney transplant exists only in affluent countries.
Even though a transplant is the best renal replacement therapy, it is available to only a fraction of CKD patients. Many end-stage patients have to choose from either of the two types of dialysis.
Peritoneal Dialysis
Many countries prefer peritoneal dialysis over hemodialysis because this procedure is simple, cheaper, and, more importantly, allows the patient to live daily without taxing too much of his time or energy.
As for all types of dialysis, a patient needs access (read tube) for performing peritoneal dialysis. Achieving this access requires a simple surgery, a small operation that involves making an inch-long incision near the belly button, to insert a plastic tube inside your tummy. One end of the tube rests inside your belly between the two layers of peritoneal membrane; the other end is taped on the surface of your stomach. This tube, the peritoneal catheter, should not be used for at least two weeks after surgery, for it takes at least that much time for the surgical site to heal and the catheter to be secure at its place of insertion. Also, keep in mind that the peritoneal catheter stays in your belly permanently.
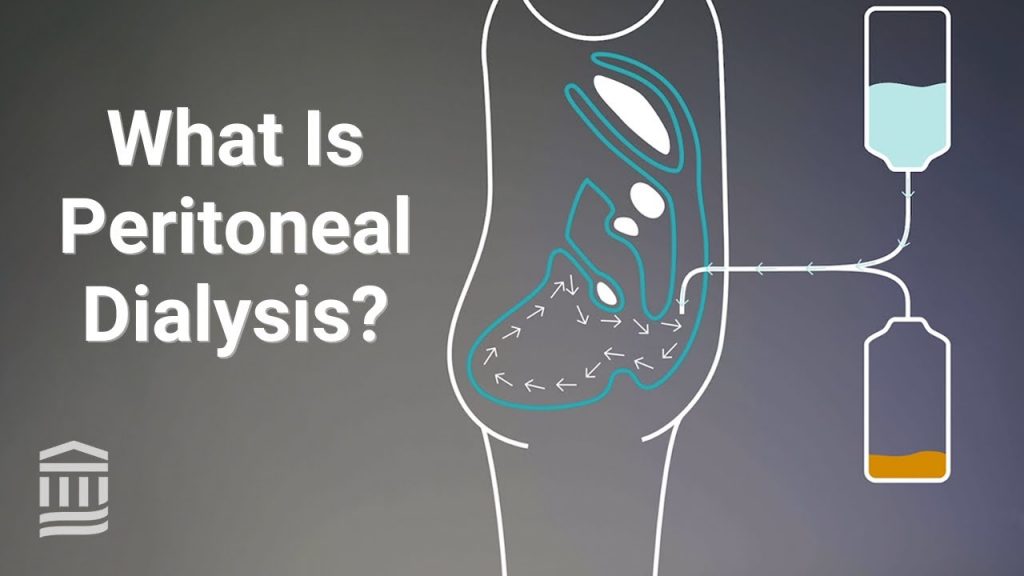
For dialysis, the patient connects the outer end of the catheter to a bag of a unique solution called the dialysate, pouring the liquid into his belly. Similarly, when it is time to drain the fluid, the patient connects the tube to a drainage bag, allowing the fluid to be drained from his belly.
In many countries, patients use a machine for peritoneal dialysis. Operating this machine is very simple—one has just to connect the device to the outer end of the peritoneal catheter. Then, while the patient is asleep, the machine does all the work, pouring the dialysate inside the belly and draining it out, repeating the process all night long. And when the patient wakes up, his dialysis for the day is already done.
However, the peritoneal dialysis machine is still a privilege and is available only in affluent countries.
Hemodialysis
Hemodialysis involves a lot of visuals of blood, hence the name hemodialysis. For hemodialysis, you need vascular access, meaning a site that allows the all-too-powerful dialysis machine to pull blood from the body, pump it through a filter, and then return the filtered blood to the body.

There are only three main types of access: An arteriovenous fistula, an arteriovenous graft, and a dialysis catheter.
An arteriovenous fistula is the best hemodialysis access—it has the longest life and the least number of complications. Creating an AV fistula involves a minor surgery at your forearm, connecting an artery and a vein. After the surgery, the connection requires six weeks to three months to mature, whereafter the dialysis staff can safely use the fistula.
For fistula surgery, a patient’s forearm blood vessels must be large enough, which, unfortunately, is not always the case. For these patients, a surgeon uses a supporting tube made of synthetic material to connect an artery and a vein.
Often, in case of emergencies or if both fistula and graft fail, a catheter is placed in the neck vein, internal jugular vein to be specific, to access blood for dialysis. However, a hemodialysis catheter has many complications, including infections and clotting.
Hemodialysis requires a patient to go to a designated dialysis center three times a week, where, on average, he spends about 5 hours each visit. You can also do hemodialysis at home using a specific machine designed for this purpose.
Take Home
Renal replacement therapy offers a kidney failure patient a second chance to live. Yet, every replacement therapy has its advantages and disadvantages. Therefore, you must choose wisely. And to make a wise choice, you should start learning about these options as early as possible.
Initially published in MinuteMirror on April 03, 2023.