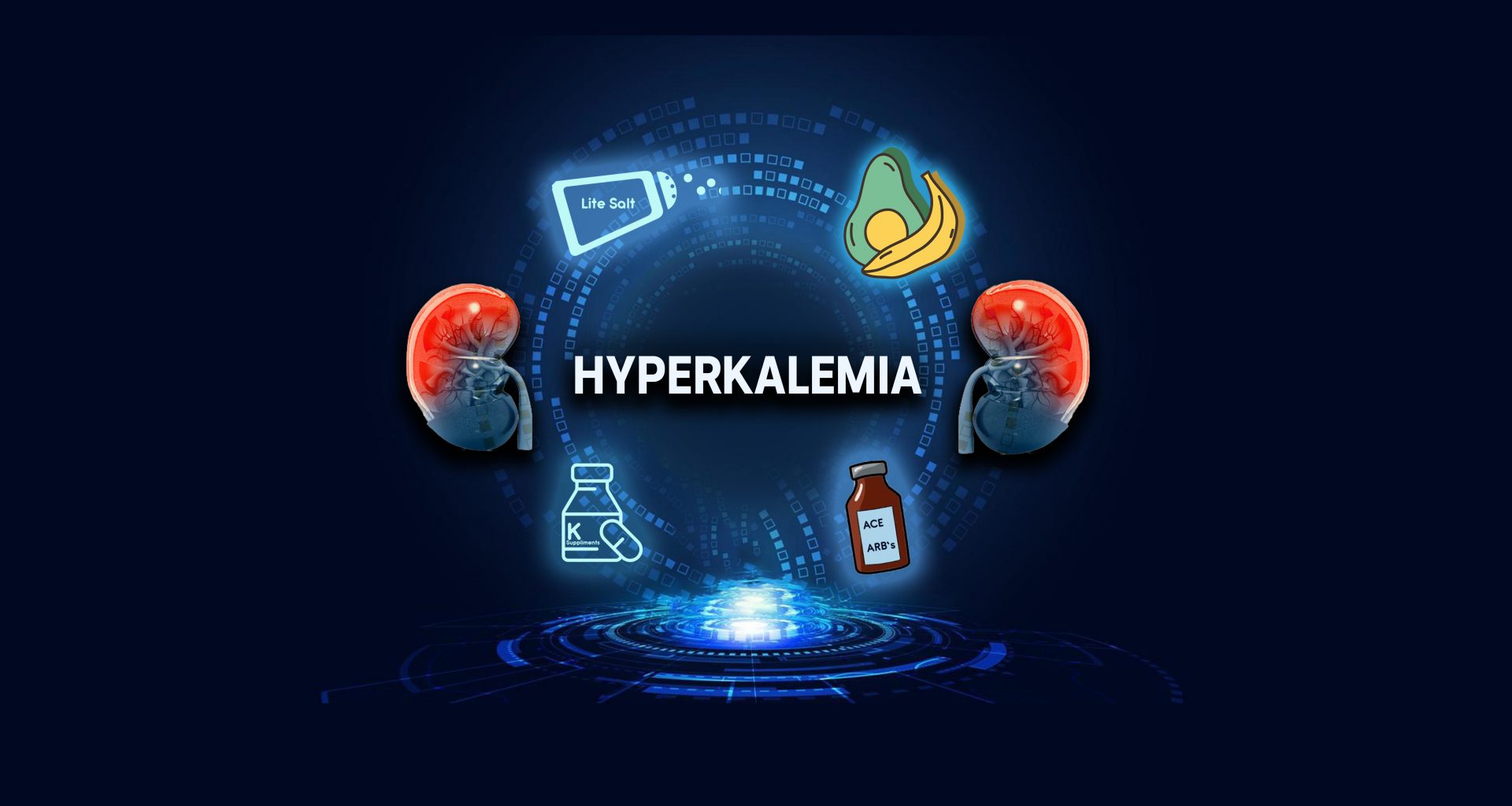
Hyperkalemia is medical jargon that means potassium level above the standard upper limit. The level between 3.6 and 5.2 is considered a normal range. Anything higher is hyperkalemia. A level between 5.2 and 6 qualifies for mild hyperkalemia, a range that will not kill you but should raise the alarm. Once the potassium level climbs over 6, a potentially lethal level, you need urgent treatment.
Hyperkalemia or high potassium level is expected in the late stages of CKD. By this time, the kidneys’ ability to dump potassium into the urine has dropped remarkably. As a result, kidneys fail to keep the potassium within the normal range.
How Kidneys Handle Potassium
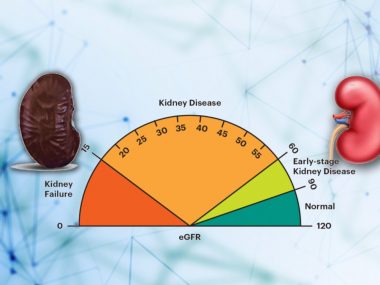
Although our body excretes some potassium via the large intestine, long-term regulation of potassium balance occurs primarily through the kidneys. Nephrons, kidneys’ filtration plants, are equipped with a potassium sensor at every turn. As soon as they detect any changes in the potassium, they activate downstream pumps that either turn potassium excretion on or off, depending on whether the blood potassium level is low or high.
As kidney disease worsens, the number of these filtration plants (Nephrons) significantly drops, making hyperkalemia a logical consequence. But it is not just that fewer nephrons are fighting against a bigger potassium load; these nephrons also now work in a less-than-optimal environment. To fine-tune the potassium excretion, kidneys need healthy nephrons, of course. But for their best performance, these nephrons require a healthy milieu, too: normal sodium level in the body, optimal fluid balance, and normal pH. None of these metrics are normal in a CKD patient, making it hard for the remaining nephrons to work optimally.
True, weak kidneys produce high potassium levels, but CKD patients have more than just the weak kidneys behind this hyperkalemia.
Causes of Hyperkalemia in CKD
High Potassium Diet

Almost all foods contain some potassium, and as far as late stage 3 of the disease, our kidneys handle this daily potassium burden very well. However, when eGFR falls below 30ml/min, potassium-rich foods become a cause for concern. These potassium-rich items need either to be completely eliminated or severely restricted. The items are listed below, and links to detailed charts are listed in the further reading. I always emphasize to my patients the importance of keeping these diet charts on their food table or cell phone, where this information is easily accessible for quick reference.
Lite Salt
To cut down their sodium intake, many CKD patients replace their regular salt with “Lite salt.” Lite Salt is a blend of equal parts of sodium and potassium chloride. Its one serving contains half the amount of sodium than regular salt, which helps reduce sodium intake; however, it has enormous amounts of potassium, which can raise your blood potassium above the normal range. While this trick of using lite salt may work well in the initial stages of CKD, it may put you at risk of hyperkalemia in the advanced stages.
Potassium Supplement
It is not uncommon to see many CKD patients using potassium supplements early in the disease. The need for potassium supplements arises due to diuretics, most of which lead to the loss of a lot of potassium in the urine, resulting in low potassium levels. Since low potassium levels are not safe, either, doctors add potassium supplements to prevent hypokalemia, meaning low blood potassium levels. However, as kidney disease trudges along the border of stage 4 and starts to lose its ability to excrete potassium, these hitherto helpful supplements accumulate in the body, causing hyperkalemia.
Potassium Sparing Diuretics
Like potassium supplements, many physicians use potassium-sparing diuretics to counter the potassium-lowering effects of strong drugs like Lasix and Bumex. Potassium-sparing diuretics act to block the excretion of potassium. Usually, this combination works well in the early stages of CKD, but in the late stages, this beneficial partnership can transform into a lethal combination. These drugs can cause fatally high levels of potassium. Therefore, the doctor checks your potassium levels a week after starting these potassium-sparing diuretics.
ACEIs and ARBs
These two classes of medicine are the most crucial tool for managing kidney disease. They slow down the loss of kidney function, adding years to your kidneys. And they work miracles for almost all stages of CKD. However, during the late stages of CKD, they increase the risk of developing hyperkalemia.
Miscellaneous Drugs
Then there is a list of commonly used drugs that lead to dangerously high potassium levels in kidney disease patients: NSAIDs (Ibuprofen), Bactrim, propranolol, and heparin (a blood thinner mainly used in hospitals).
Symptoms of Hyperkalemia
Potassium plays a pivotal role in generating an electric current in the body. Consequently, hyperkalemia interferes with the electrical circuitry of the heart and muscles, two organs that require a continuous supply of current for optimal performance. In the muscles, high potassium causes weakness or cramps. Some patients even complain of numbness, tingling, or burning in their hands and feet. For the heart, above-normal potassium proves more perilous. At slightly higher potassium levels of 6 or more, the heart either slows down or becomes too excited. However, at levels above 7, the electric board of the heart can have a short circuit, generating lethal arrhythmias at any minute. This is particularly true with sudden changes in potassium levels.
Management of Hyperkalemia
Low Potassium Diet
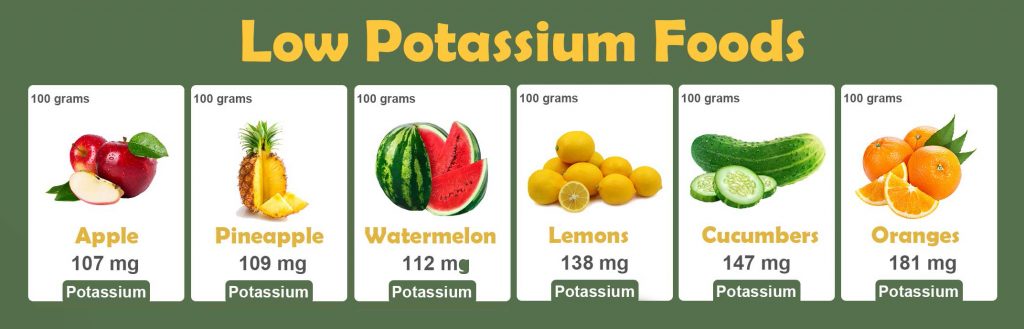
A low-potassium diet is the easiest thing to prescribe, which is why most doctors consider it the first line of defense against hyperkalemia. A low-potassium diet means a dietary intake of fewer than 3000 mg of potassium daily. To achieve this goal, you need to cut down the intake of potassium-rich foods and use instead items that are not so packed with potassium. But you still have to watch your serving. A large serving of a low-potassium diet can easily trip you over into hyperkalemia.
A low-potassium diet might look like the easiest choice to physicians, but it creates considerable confusion for the patient. Counting milligrams of potassium in every bite is more challenging than it sounds. As a result, many patients even give up on fruits, vegetables, and spices—the three most healthy foods on planet earth.
Therefore, in my practice, the recommendation to reduce the potassium intake comes last, after I have taken care of the most common causes of hyperkalemia.
Manage Your Medications
Some medications, such as ACEIs and ARBs, are the cornerstone of CKD management. They must stay. Yet, you can counter drug-induced hyperkalemia by using another group of drugs that are equally important in the management of kidney disease but possess potassium-lowering properties. Lasix is one; another is hydrochlorothiazide. Both diuretics, commonly used to treat high blood pressure and volume overload in CKD patients, pair very well with ACIs or ARBs, forming a combination that protects kidneys and averts hyperkalemia.
Similarly, potassium-sparing diuretics, such as Aldactone and Eplerenone, should always be combined with loop diuretics like Lasix and Bumex.
Scrutinize Your Supplements
As discussed above, the savior potassium supplements, so helpful in the early stages of kidney disease, can often become the source of hyperkalemia in advanced CKD. It is time you dropped them. Likewise, remove the lite salt from your diet. Rarely, a few multivitamins or other alien-sounding supplements contain high amounts of potassium. A normally functioning kidney may not have difficulty processing these supplements’ potassium content, but it might be overwhelming for a weak kidney. Next time, remember to read the supplement label specifically for the amount of potassium per serving.
Sodium Bicarbonate
No late stags CKD prescription can be complete without sodium bicarbonate. With the decreasing ability of the kidney to dump acids into the urine, acids start to build up in the blood, necessitating the use of the antiacid—sodium bicarbonate. Besides balancing the acid level, sodium bicarbonate helps lower potassium levels. So, check your serum bicarbonate; if it is low, ask your physician about sodium bicarbonate.
Washing, Rinsing, Leeching, Boiling
Washing and rinsing are a must for canned foods because these items are rich in both potassium and phosphorus. Therefore, preferably, CKD patients should stay away from canned foods. However, if they cannot avoid canned foods, they should go over the following ritual. First, drain all the juice in the can; next, rinse the food item in fresh water and drain the rinse water; then, rinse it a couple more times to wash off all the preservatives.
For the foods that you like and cannot imagine parting with, you can use leaching. Leaching is a process where you soak your favorite fruit or vegetable in fresh water for two hours, then drain the water and use the food item. During the two hours of leaching, the concept goes, water pulls the potassium out of the food item, lowering the potassium content per serving. However, leaching by no means makes the food potassium free. The leached fruit or vegetable still retains a considerable quantity of potassium, demanding caution.
Lastly, some nephrologist chuckle when you ask them about leaching. These hard-core practitioners believe more in the process of boiling. Boiling is another recommended method for potassium removal, and, according to some research, more potent than leaching.