A patient with chronic kidney disease cannot be said to know his illness well unless he masters these ten concepts that form the foundation of excellent kidney disease management.
I call this knowledge “A patient’s kidney disease awareness.” To reduce the burden of kidney disease in the world, we need awareness of this invisible illness at multiple levels—at the global level, at the national level, at the healthcare level, and most notably at the patient level. This blog concerns the last level—a patient’s awareness about his kidney disease.
Rather than starting from the screening of kidney disease, this blog assumes that the patient already knows about his kidney disease.
Diagnosis—What is the cause of the kidney disease?
Just learning that you have kidney disease will only do a little if you plan to perfect your kidney care. Why? Because chronic kidney disease is not an illness in itself. CKD basically refers to less-than-normal-functioning kidneys that could result from many different conditions—diseases that irreversibly damage the kidney tissue over time. Therefore, it is essential to learn what has caused your kidney disease. For example, high blood pressure and diabetes account for about seventy percent of the cases of chronic kidney disease, and chances are that one of them is the culprit in your case. Other causes of CKD include heart and liver disease, drugs and toxins, cystic kidney disease and autoimmune disorders.
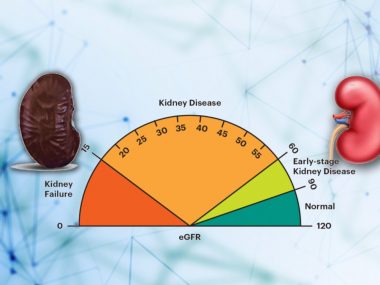
Staging—Where does your kidney function stand?
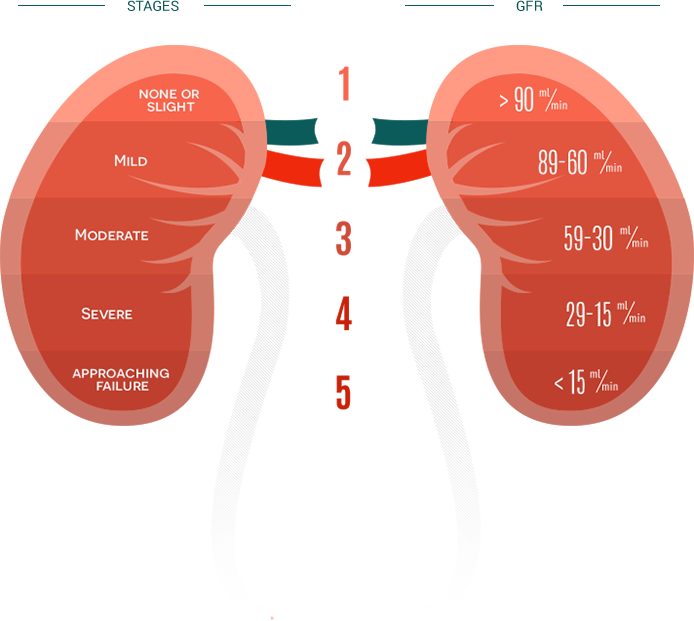
After diagnosis, it is crucial to learn how much functioning ability the kidneys have lost. Doctors measure the functioning level of your kidneys by calculating their filtration capacity—thus the name glomerular filtration rate, commonly known as eGFR. Calculating eGFR requires your age, gender, and blood creatinine level, punching which numbers in a specific equation gives the value in milliliters/min. Normal eGFR is 90ml/min or above. Anything below 90 ml/min is considered chronic kidney disease. Doctors divide kidney disease into five stages based on eGFR (See table below). Stage 1 means normal kidney function, 2 indicates some abnormality, three suggests early kidney disease, four is advanced, and five is the last stage.
Proteinuria—How much protein are you spilling in the urine?
Proteinuria portends poor CKD outcomes. In fact, proteinuria is the single most important determinant of rapidly declining kidney function. Consequently, the guideline makers placed proteinuria along with eGFR for a better picture of the kidneys’ condition at any given moment. The resulting pictorial is called the heat map. On this map, green means good and red raises alarm.
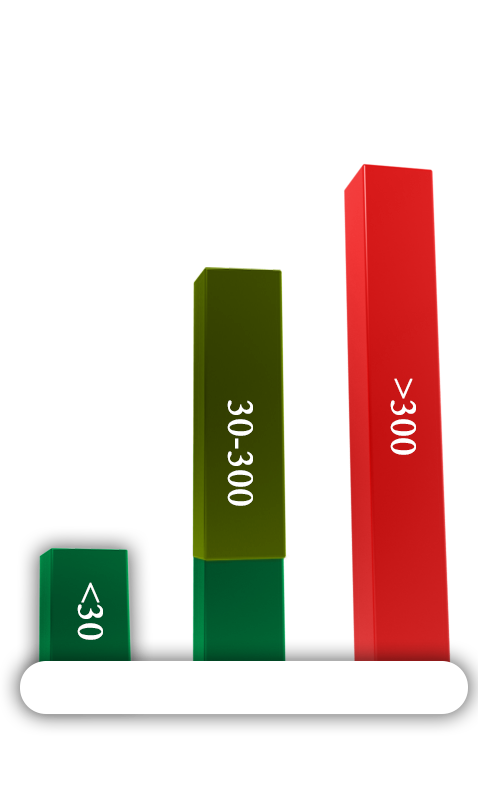
Every CKD patient must have his urine checked for protein. This screening starts with a simple urinalysis, and if the urine is positive for proteins, your doctor quantifies the protein in the urine with another urine test called protein-to-creatinine ratio. Normal urine protein is less than 30. A value between 30 and 300 means moderate proteinuria. A value above 300 is considered severe proteinuria.
Trajectory—How rapidly your kidney function is declining?
Usually, a chronic kidney disease patient should follow up with the kidney disease specialist at least twice a year, more often in some cases. The purpose of these follow-ups is to chart your disease progression. On these visits, your doctor basically checks your kidney function—eGFR and proteinuria—and makes a graph that allows him to gauge the progression of your disease. In a patient with well-managed kidney disease, eGFR should not fall more than 2 ml/min per year. If your eGFR falls between 2 and 5 ml/min per year, your kidney disease is poorly managed. And if your eGFR is declining more than 5 ml/min every year, it is called rapidly declining kidney function—a nightmare.
Tracking the kidney function helps you and your healthcare team optimize your kidney disease management.
Note: In the advanced stages of kidney disease, a patient often requires frequent visits—almost once a month—and gets many more tests done besides creatinine and urine protein. We will discuss such patients in a separate blog post.
Lifestyle—What do you need to eat, drink, and do?
Lifestyle refers not to any one thing; it is rather a combination of behaviors—minor daily routines that compound to give your kidney function—or your overall health, for that matter—a boost.

Let’s start with food. A healthy diet forms the foundation of a healthy lifestyle. As far as the kidney is concerned, in the early stages of the disease, the definition of a healthy diet remains the same as it does for the general population: unrefined carbs, balanced use of proteins, unsaturated fats, and a lot of fibers using fresh fruits and vegetables. However, in the advanced stages of kidney disease, dietary restrictions demand arduous changes in the diet, particularly in the intake of sodium, potassium, and phosphorus.
Other major pillars of a healthy lifestyle are regular exercise—30 to 45 min moderate intensity workout daily— and decent sleep—7 to 9 hours every night. Then, you must quit smoking or other recreational drugs that directly hurt the kidney, such as cocaine.
Comorbidities—Do You Have Other Illnesses?
CKD patients almost always carry other conditions, too, such as diabetes, high blood pressure, and heart disease. These conditions can be either the cause of kidney disease or just happen to be there while you got the kidney disease from something else entirely, say, for instance, an autoimmune disorder or a medication’s side effect. Regardless, optimal treatment of these conditions is inevitable for slowing doing the progression of kidney disease.
And for the optimal management of these co-existing conditions, a kidney disease patient must know what the blood pressure and diabetes goals for a CKD patient are.
Complications of CKD—Anemia and Acidosis
In the advanced stages of kidney disease, as kidneys lose more function, their ability to handle the body’s waste products declines, one adverse effect of which is increased acidity in the blood. This condition is called metabolic acidosis. Acidosis is not only a marker of advanced CKD; it also worsens kidney disease. Luckily, mitigating acidosis slows down the progression of kidney disease. To achieve this goal, your kidney doctor prescribes sodium bicarbonate pills three times a day, with a target serum bicarbonate (HCO3) level of 22 or above.
Around the same time when acidosis appears, another complication of kidney disease that becomes prominent is anemia—a lack of red blood cells, indicated by low hemoglobin. Anemia in CKD accrues primarily from low erythropoietin production by the kidney, a hormone that stimulates bone marrow to produce hemoglobin and red blood cells. However, lack of iron—also due to CKD-induced inflammation in the body—also plays an important role. The treatment, therefore, consists of both iron supplements (in the early stages) and synthetic erythropoietin (in the advanced stages).
Medications—What to take and what to avoid?
All chronic kidney disease patients must be aware of two groups of medicines: kidney-protective and kidney-damaging.
Kidney-Protective Medicines
Every kidney disease patient is unique because every CKD patient has a unique set of conditions that vary from other kidney disease patients. For example, one patient may have diabetes and kidney disease only, while another patient may have diabetes, high blood pressure, and even heart disease.
Likewise, their prescriptions also differ from each other, depending upon a patient’s associated conditions. Yet, some medicines benefit kidney disease regardless of the underlying cause and accompanying illnesses. One such group of drugs is ACIs (Angiotensin-converting enzyme inhibitors), including medications like Lisinopril and Benazepril. Another group is ARBS (Angiotensin receptor blockers), medicines like Losartan and Valsartan. Most recently, Flozins appeared as a new kid on the block and aced all positive outcomes one could imagine.
In almost all cases, based on your condition, these kidney-beneficial drugs can be easily used alone or in combination. On your next visit, don’t forget to ask your doctor about these drugs.
Kidney-Damaging Drugs
This group ranges from completely contraindicated medicines to compounds that should be used cautiously and only when there is no way around it.

Painkillers like Ibuprofen and naproxen should be avoided at all costs, for these drugs not only directly damage your kidney, they also worsen other conditions like heart failure and gastric ulcer.
On the other end of the spectrum, there are drugs known to damage the kidney directly, yet a CKD patient can use them under the strict supervision of a doctor, preferably a kidney disease specialist. Dyes used in imaging studies and a few antibiotics fall in this category.
Risk of Dialysis—A Look into the Crystal Ball
We now have some equations that can tell how your kidney disease would do tomorrow based on how your kidney disease is doing today—a look into a statistical crystal ball. These equations are modern equivalents of soothsayers but with one difference—they use data as their primary source of information, compared to soothsayers whose prediction relies totally on intuition.
The risk stratification equations project your chance of going on dialysis in the next two years and five years. We also have an equation that can even tell your chance of dying from other conditions like a heart attack before ever needing dialysis. Well, many kidney disease patients regard these formulas as nothing more than a doomsayer, heralding a pending calamity; however, wiser patients use these predictions with prudence, to set not only their kidney disease goals but also straighten out their financial, social, and spiritual matters.
Renal Replacement Therapy
Lastly, as a kidney disease patient, you must know when to get ready for renal replacement therapy. In countries with affluent healthcare, the kidney team arranges Kidney Smart classes for all patients with stage four CKD, meaning when the eGFR falls below 30 ml/min. Among many other things, these classes discuss renal replacement therapy and its logistics.
Renal replacement therapy refers to any mechanism that replaces the function of native kidneys. It includes kidney transplant, hemodialysis, and peritoneal dialysis. During Kidney Smart classes, the patient learns about various modalities for dialysis and how they work. This information allows patients to select a modality that fits their personality.
Take Home
If there is only one thing you can take from this blog, it should be this one—no single ingredient can save your kidneys. Kidney care requires a full recipe. The more you learn about your kidney disease, the better you get at managing your CKD. Learning the ten essentials discussed in this blog can help you easily navigate your kidney disease.