Kidney health and general health go hand in hand. In order to maintain good kidney function, it is imperative to monitor metabolic health. You can assess your general metabolic health with the help of a few basic tests. All doctors regularly do these tests; yours might have done them for you as well but never cared to explain their actual worth. Let’s discuss basic tests for monitoring metabolic health in a kidney disease patient.
Complete Blood Count (CBC)
This test has many uses, both in acute and chronic diseases. As for kidney disease patients, this lab primarily gives us information about anemia, meaning hemoglobin deficiency or, in layman’s language, low blood levels. Low hemoglobin in kidney disease patients can be due to a deficiency of either iron or vitamin B12 or both, confirmation of which then requires specific tests discussed below.
Basic Metabolic Profile (BMP)
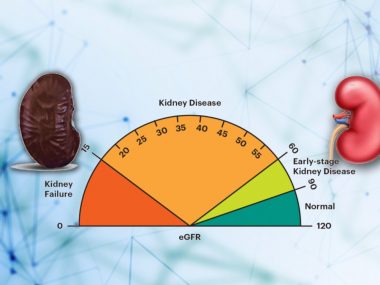
This test includes a group of tests: kidney function tests, including blood creatinine, urea, urea nitrogen, and collection of serum electrolytes, including sodium, potassium, chloride, bicarbonate, and calcium. All of these tests are vital for a kidney disease patient. Creatinine is required to confirm the diagnosis and staging of kidney disease; urea and blood urea nitrogen act as guides to start dialysis; derangement of electrolytes indicates poor kidney function as well as dietary delinquency. Calcium is important in particular, for a high calcium level can point to an illness arising from elsewhere—the potential cause of kidney disease.
Comprehensive Metabolic Profile (CMP)
Adding liver-related tests to the basic metabolic profile gives you an even broader picture of your health, hence called the comprehensive metabolic profile. Among liver tests, one that directly concerns kidneys is albumin. Among many things that can reduce blood albumin, one is nephrotic syndrome, meaning the loss of more than three grams of albumin in the urine—a serious kidney condition that calls for immediate attention.
Indirectly, CMP can help identify fatty liver and, thus, metabolic syndrome by showing elevated levels of liver markers, particularly alanine aminotransferase (ALT) and aspartate aminotransferase (AST). Metabolic syndrome implies insulin resistance—the root cause for all metabolic disturbances in the body, including damage to the inner lining of kidney blood vessels.
Lipid Profile
This test has many components, varying from country to country and lab to lab. Regardless, this test can be viewed in two ways. In the traditional view, the doctor looks at individual parts of the lipid profile and prescribes the medicine to fix that number. For instance, if LDL (Low-density lipoproteins) is high, they give statins, cholesterol-lowering medicine; for high triglycerides, they have fenofibrate; for low HDL (High-density lipoproteins), they may add niacin.
A broader, more holistic metabolic view holds that abnormalities of various parts of the lipid profile stem from the same source—an unhealthy lifestyle and ensuing metabolic disturbances. Accordingly, the focus of management should primarily be on the cause—unhealthy lifestyle, and not the individual values—LDL, HDL, and triglycerides. This does not mean at all that medicines are of no use at all, nor does this view exclude the role of genes in regulating our cholesterols. This metabolic view maintains that the treatment of abnormal cholesterols must start with lifestyle changes, and medicine should be added only if necessary.
Uric Acid
Just like cholesterols, uric acid as a blood test has also undergone a paradigm shift. No longer considered just a by-product of purine metabolism, uric acid is now increasingly recognized as a marker of inflammation and insulin resistance, that is, poor metabolic health. As regards the kidneys, uric acid has a two-way relationship: poorly functioning kidneys build up uric acid in the body, while high uric acid levels can hurt the kidneys.
Management of uric acid should start with lifestyle modification. If the level remains high despite these health changes, some nephrologists prefer to start a medicine to bring it down within the normal range.
Hemoglobin A1c (HbA1c)
Consider this test as a glance at your daily average blood sugar for the past three months. Despite its limitations, hemoglobinA1c has become a standard test for diagnosing and managing diabetes. Currently, the normal value is set at 5.3% or below; 5.7 to 6.4% is considered pre-diabetes; and 6.5% and above means diabetes. All newly diagnosed kidney disease patients should get Hemoglobin A1c checked, for diabetes is the most common cause of kidney disease.
Diabetes implies extremely poor metabolic health and should be strictly managed. The recommended target HbA1c for diabetic kidney disease patients is below 7% using medication. I recommend trying a complete reversal of diabetes with a healthy lifestyle, aiming for HbA1c of no less than 5.3%, potentially allowing one to be off all diabetes-related medicines.
HOMA IR (Homeostatic model assessment for insulin resistance)
HOMA IR is an indirect, cheap, and more practical way of measuring insulin resistance, the root cause of poor metabolic health. It involves measuring fasting blood glucose and insulin levels, which are then punched in an equation to calculate insulin resistance. The cut-off value is 2; anything above that suggests insulin resistance.
I have a very high threshold for doing HOMA IR, reserving it only for those who have borderline blood pressure, weight, and cholesterols. For such patients who assume themselves to be very healthy, HOMA IR offers a reality check, helping them to dispel their illusion of health.
Urinalysis
A full workup of a kidney disease patient is incomplete without urinalysis. Far from being a filthy fluid, urine provides a window to look inside the body, even though not a fancy one, I admit. Its color, consistency, smell, cells, and chemical values—all play a crucial role in assessing kidney disease. Among these components of urine, the most important for diagnostic purpose are red cells and protein. The presence of any of the two escalates things to an alarming level, requiring immediate attention and further evaluation.
Vitamins
Kidney disease patients, owing to the nature of the disease, are prone to some nutritional deficiencies. They easily develop a deficiency of Vitamin D, Vitamin B12, and iron, particularly in the late stages of the disease. Having these values checked once or twice a year can fend off unnecessary suffering from vague symptoms, such as restless legs and lassitude.
Hormones
Kidney disease, along with other changes in the body, causes alterations in many hormones. Three of these hormones require regular monitoring, especially if a patient feels tired and unwell. The most important is the parathyroid hormone. In kidney disease patients, the body dials up the secretion of parathyroid hormone to keep the phosphorus level in the normal range. A very high level of parathyroid hormone means poor phosphorus balance, pointing to the fact that the patient is taking excessive phosphorus intake. Other common hormonal systems that can be disturbed in kidney disease are thyroid and sex hormones.
Summary
These ten tests allow you and your doctor to gauge your general health, allowing you to make necessary adjustments to enjoy better general and kidney health.