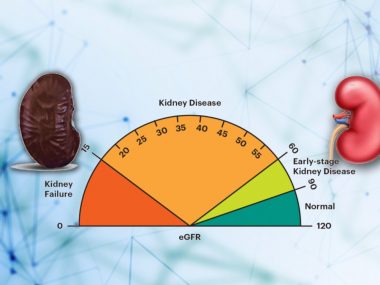
Only a kidney disease patient can tell the worth of kidney function; the rest of us take it for granted. These patients would do anything to hear that their kidney function could get better. While this reverse in kidney function is not possible for patients with chronic kidney disease, kidney function can recover significantly, and often wholly, in patients with Acute Kidney Injury. Therefore, whether you have chronic kidney disease or not, if you see a new drop in your kidney function, discuss the following causes of reversible decline in kidney function with your doctor. I always stress to my patients and students to look for a recovery in kidney function, even in dialysis patients.
Note: Kidney function is measured as Glomerular Filtration Rate or GFR. So, you may see these terms used synonymously throughout this blog.
Dehydration—or Loss of Fluids in the Body
The network of blood vessels in our body contains about 5 liters of blood at any given time. The blood has many components, but two are essential for kidney function: the fluid part called plasma, and red blood cells. If any of these two get too low, your kidney function may drop. Common causes of a decrease in plasma level are decreased fluid intake, excessive sweating, vomiting, and diarrhea. On the other hand, both plasma and red blood cells drop when a patient bleeds.
In most cases of dehydration, drinking extra fluids is sufficient. In severe cases, however, patients may need to go to a hospital to get intravenous fluids. Regardless, a dehydrated patient is likely to fully recover and rarely needs dialysis. Yet, if dehydration is prolonged enough, it can lead to a specific type of injury called Acute Tubular Necrosis (We will discuss in future blogs).
Medications
Some medications can cause a drop in kidney function, usually a temporary decline that recovers after stopping the drug. Still, this drop can be permanent if timely measures are not taken. The impact of medication on kidney function is most prominent when you are dehydrated. So what should you know about these medications?
ACEIs and ARBs
Medications from both these groups are vital for kidney disease patients. Even though they are blood pressure medications, their benefits go beyond controlling blood pressure: they particularly ease the pressure dynamics in the blood vessels inside the kidney, protecting the renal function from long-term damage.
However, a slight drop in kidney function is commonly expected after their initial use, a trade-off that helps delay or may even prevent a future need for dialysis. To prevent a drop in kidney function from ACEIs/ARBs, the best strategy is to hold off using other medications like painkillers and stay well hydrated. ACEIs medications usually come with -pril at the end of their names, as in Lisinopril and Ramipril. ARBs typically end with -tan, like losartan and Valsartan.
Painkillers (NSAIDs)
Pain medications that belong to this group, commonly called NSAIDs, including Motrin and Naproxen, drop GFR by decreasing blood flow to the kidneys. This side effect is more marked in those patients who are dehydrated, taking ACEIs/ARBs, and/or have heart and liver failure.
Always talk to your doctor before using any over-the-counter medications, particularly pain medications. Remember that kidney is the final drain for all the chemicals that enter your body, a meeting place where different drugs can cross-react.
Other Medications
Many show concern about the safety profile of Aspirin in CKD. First, Aspirin should not be used as a pain relief medication because it increases the risk of bleeding. However, the low dose of Aspirin, 81 to 162 mg, used in heart and stroke patients, is okay to use, even in patients with reduced kidney function.
Another commonly asked medication is Proton Pump Inhibitors, a few examples of which are Omeprazole, Pantoprazole, and Lansoprazole. Some studies have shown that these drugs adversely affect the kidneys, while others reveal no such evidence. Anyways, these reflux drugs should be avoided in CKD patients.
Dyes Used in Radiology
Sometimes, CT scans require an intravenous dye, commonly called IV contrast, for better images. Unfortunately, this contrast may temporarily or permanently worsen your kidney function. The newer contrasts have a better safety profile, however. Still, a kidney disease patient should only go for such a test after talking to his nephrologist.
Blockage of Urine Flow
Each kidney pours its urine into a narrow pipe called the ureter. Both ureters drain into the bladder. The urine then comes out of the body through the urethra. Any obstacle on this pathway can hamper the urine flow, leading to back pressure in the kidneys and a decline in their function.
One common cause of such obstruction is an enlarged Prostate, a common problem in older patients. Decreased kidney function in such cases is reversible and resolves completely once the prostate is taken care of.
When they obstruct both ureters, kidney stones can cause similar problems and need timely removal to prevent permanent kidney damage.
Reversible Kidney Function After Starting Dialysis
While getting off dialysis in patients with chronic kidney disease and permanent kidney damage is not possible, such recovery is common for patients with acute kidney injury. Therefore, if you develop an acute kidney injury that requires dialysis, always ask your physician about the chances of getting off dialysis.
It so often happens that dialysis patients and their medical records, due to lack of continuity in care, are hard to keep track of. As a result, physicians fail to recognize that these patients’ kidney function needs close monitoring to look for recovery. Many patients stay on dialysis just because someone forgot to punch in the correct diagnosis.