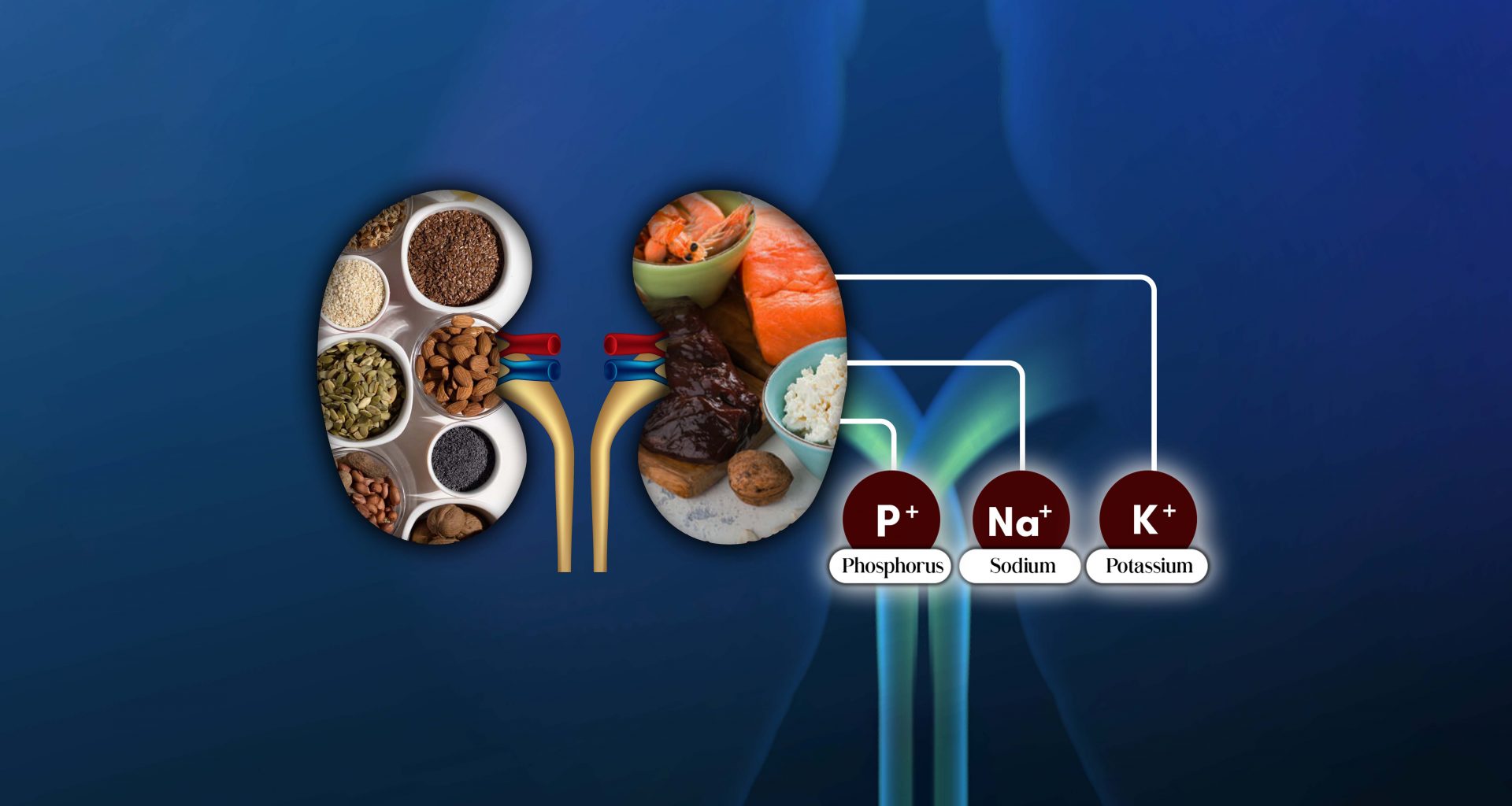
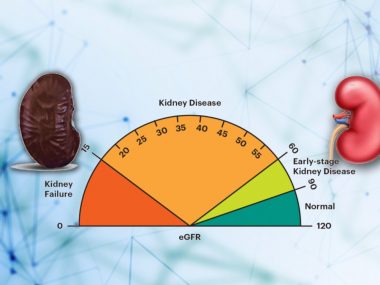
A kidney diet demands severe dietary restrictions in its late stages. As a kidney disease patient enters stages 4 and 5, the kidneys’ ability to regulate certain salts starts to falter.
Consequently, a kidney diet in the advanced stages of CKD requires decreasing the intake of the salts like sodium, potassium, and phosphorus, significantly limiting the foods one can enjoy. However, by understanding the dynamics of these salts in the body and their quantity in various foods, one can meet the restrictions without feeling limited. That is what we will seek to do in today’s blog.
Smooth Landing on the land of limitations
If you have been a conscientious kidney disease patient from the beginning, following your medical and dietary instructions religiously, two things will happen. First, you have brought down the risk of entering the late stages to a minimum (you can calculate this risk but more on it in future blogs). Second, you have become a pro in reading your food labels and applying these instructions to your diet. Consequently, if you ever reach advanced kidney disease, you will navigate this territory smoothly.
Let’s find out what perils lay there and how to deal with them.
Sodium—Backbone of A Kidney Diet
Recommended salt intake in all stages of CKD is 4.5 grams (sodium 2.3 grams) or below a day. However, patients with advanced kidney disease or on dialysis may need more titration.
Recommended salt intake in all stages of CKD is 4.5 grams (sodium 2.3 grams) or below a day.
A high salt intake is bad: it raises your blood pressure, increases the risk of stroke, heart attack, and heart failure, and may play a role in worsening atherosclerosis. For a patient with kidney disease, sprinkling salt on the food is like spraying propane on a lightly burning stove. Stop doing it.
When you cut down your salt intake as a part of your kidney diet, it improves your blood pressure. Additionally, low salt intake augments the efficacy of certain blood pressure medicines called ACEIs and ARBs, often requiring a decrease in the dose of other blood pressure medicines.
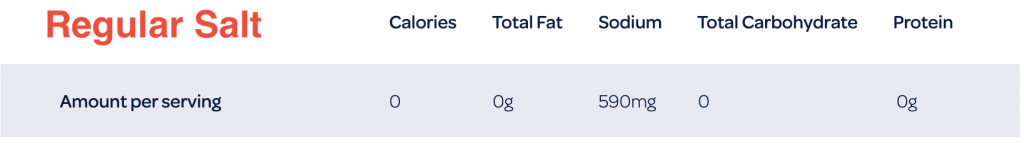
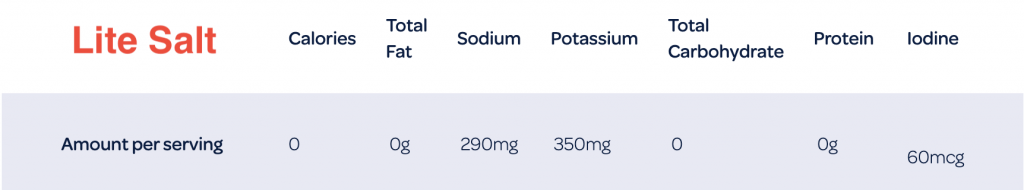
Caution: Many patients, in an effort to reduce their sodium intake, replace regular salt with “Lite Salt.” Lite Salt is a blend of equal parts of sodium and potassium chloride. Its one serving contains half the amount of sodium than regular salt, which helps reduce sodium intake; however, it has enormous amounts of potassium, which can spike your blood potassium above safe levels.
Potassium—How Much is Too Much
The recommended potassium for advanced kidney disease patients is less than 3000 mg daily.
The recommended potassium for advanced kidney disease patients is less than 3000 mg daily.
As patients advance into the late stages of kidney disease, potassium management becomes a huge challenge. By now, kidneys have failed to regulate the potassium we get from our regular diet. Then, medications like ACEIs/ARBs, a lifeline for CKD patients, tend to raise blood potassium levels. Worse, many patients can’t even use common medicines, such as ibuprofen and some antibiotics, without messing with the potassium in their blood. Lastly, many kidney disease patients replace their regular salt with Lite Salt, thus ingesting large amounts of potassium unknowingly.
You can use several tricks to manage your potassium level (I will discuss them in the blog on potassium), but the first and easiest life of defense is a low-potassium diet. A food is considered low potassium if its 100 grams contains about 100 mg of potassium, whereas foods with 300 mg of potassium per 100 grams qualify as potassium-rich. Still, this is a rough estimate, and I always recommend that my patients keep food charts on their table or cell, making it easier for a quick reference. Over time, many patients simply remember what foods to avoid to keep potassium levels within range.
Alarm! Potassium levels can take a plunge on the low side, too. Hence, regular follow up with your doctor and blood tests are essential because a low potassium level is not safe, either.
Phosphorus—A Kidney Diet is a Good Start
The daily recommended phosphorus intake for CKD stage 4 and 5 patients is 800 to 1000 mg. However, this amount can vary based on your blood tests: phosphorus, calcium, and parathyroid hormone level.
The daily recommended phosphorus intake for CKD stage 4 and 5 patients is 800 to 1000 mg.
High potassium is often challenging, yet it is a decently manageable issue. Moreover, any disturbance in potassium does not affect other hormonal algorithms. Phosphorus plays, however, a central role in a cascade of hormones that ensure the health of our bones. Naturally, when weak kidneys fail to excrete phosphorus, it accumulates in the body, disturbing the hormonal balance, which, in turn, leads to harmful changes in the bones and blood vessels. There is a fancy medical term for this stir-up in the body—Metabolic Bone Disease.
Phosphorus management starts with a low-phosphorus diet. Phosphorus is a common preservative, added to many foods for flavor, color, and prolonged shelf life. In short, a kidney disease patient must decrease or eliminate frozen and packaged foods, processed meat, cold cuts, and canned items. Other common foods that contain high phosphorus include dark beverages (coca cola), chocolate, dairy products, and nuts.
The Takeaway—You Don’t Have to Lose Hope or Flavor
Restricting your foods to manage the electrolytes is essential. Still, these restrictions of a kidney diet don’t mean you have to miss out on flavor. By carefully watching your symptoms and blood tests, you can enjoy all the foods in moderation. Additionally, with a low-salt diet, you can use other products to spice up your food and make up for the lost taste. At any rate, stick with the diet plan given by your doctor and always take him into the loop before starting any such product.