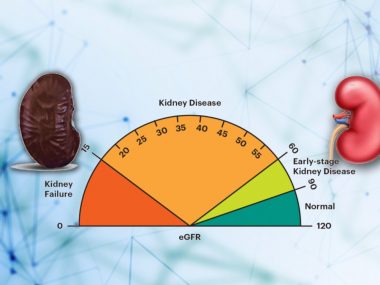
Humans learned about kidney disease long ago, but its link with blood creatinine levels came to light only in the 1940s. For the next fifty years, kidney disease management saw only two breakthroughs—dialysis and kidney transplant—both being renal replacement therapies, not preventions or treatments. It was not until 1981 that Captopril, an angiotensin-converting enzyme inhibitor, was approved by the FDA, and it took another decade to realize the benefits of these blood pressure drugs for kidney health. For the last twenty years, we have barely seen any additions to the toolbox of kidney disease treatment. However, since 2015, stars have now seemed to align in favor of kidney disease patients. Starting from a trial on Empagliflozin, a diabetes medicine that has also shown promise for many other conditions, we saw study after study about newer kidney-protecting drugs, pouring evidence that, yes, we can slow down the progression of kidney disease. In March 2024, medical science made another leap forward and successfully transplanted a pig’s kidney into a human. Besides, we now have more than ever research-based knowledge about diet’s role in kidney health. The future of kidney disease management is bright.
Two Drugs for Two Decades
When the FDA first approved captopril in 1981, its intended use was blood pressure control. Over time, however, this and other similar drugs showed benefits for patients with a weak heart. Later, many studies confirmed these clinical observations. Slowly, over the years, we learned that drugs like captopril also reduce proteinuria in diabetic patients, slowing down the progression of kidney disease. Then, it took the FDA another decade to approve the first Angiotensin Receptor Blocker in 1995, adding another class of drugs for kidney patients who were, for one reason or another, unable to use angiotensin convey enzyme inhibitors. Since then, these two drugs—angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers—have established themselves as the cornerstone of kidney disease management. While these kidney-protective drugs helped doctors save many kidneys, that was it: patients who developed side effects from these drugs, and their doctors, had nothing else to fall back on but hope.
Flozins—A Giant Leap Forward
Their hopes turned into reality when emerged on the horizon Empagliflozin. Empagliflozin belongs to a class of drugs called -flozins or, more commonly, SGLT2-inhibitors, due to the fact that they inhibit the activity of a receptor SLGT2 in the kidney. SGLT2-inhbitors have always been considered diabetic drugs because they improve blood sugar levels by excreting it in the urine. However, when scientists were doing research on Empagliflozin for its safety in heart patients, they noted not only jaw-dropping improvements in the outcomes of heart disease but also strong signals for kidney outcomes—a significant reduction of proteinuria and slowing down of kidney disease progression. Although this research was not primarily studying kidney disease patients, yet the kidney-related benefits seen in this study ushered in a new era, prompting a series of trials that would change kidney care forever.

In this new era, one trial after another confirmed the fact that kidney disease can be slowed down. The first -flozin research done primarily for kidney patients was CREDENCE, a study of diabetic kidney disease patients which proved that Canagliflozin, another SGLT2-inhibitor, slows down the progression of kidney disease in patients with diabetes who have proteinuria. This study was followed by another, DAPA-CKD, a trial that proved the kidney-saving benefits of Dapagliflozin in patients with any proteinuric kidney disease, not just diabetes. Then, came the final punch with Empagliflozin research, which shattered remaining skepticism, proving that -flozins are the ultimate kidney-protective drugs, regardless of whether the kidney disease stems from diabetes or not, or has proteinuria or not.
Keep in mind that all these benefits of SGLT2 inhibitors were over and above the benefits of the previous pair of drugs(angiotensin-converting enzyme inhibitors and angiotensin receptor blockers). This fact entails that the new sugar-controlling pills are not a replacement for the past pro drugs but an addition to the toolbox of nephrologists, one more drug to control proteinuria and slow down the progression of kidney disease. Note also that the benefits of -flozins go beyond just proteinuria and kidney function, significantly improving heart and blood vessel health and reducing a patient’s chance of hospital admissions.
In the five years between 2015 and 2020, multiple research studies ratified these results, making SGLT2-inhibitors a permanent member of the kidney cure club. While many in the medical field still shook their head in disbelief, and some in denial, new research announced another medicine to have a meaningful role in kidney disease management.
Finerenone—An Old Drug But A New Formula
The medicine was Finerenone, a new drug from an old group of medications called mineralocorticoid receptor antagonists. Nephrologists have always used drugs from this group—Aldactone and Eplerenone—for many conditions, knowing very well that these drugs reduce proteinuria. However, their use remained limited due to the side effects, particularly high blood potassium, one that made these drugs almost impossible to use in kidney disease patients who were already on angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers. For such patients, adding Aldactone was impossible without using potassium-lowering drugs, an unwelcome fix, and many patients refused.
Finerenone solved the problem. Certain attributes of the drug—short half-life, minimal active metabolites, balanced heart-kidney distribution, selective receptor blockade, and distinct gene activation—allow this drug to deliver all heart and kidney benefits without increasing potassium levels, making it a favorite mineralocorticoid receptor antagonist for cardiologists, endocrinologists—and nephrologists alike. Now, nephrologists ostentatiously prescribe finerenone to their kidney disease patients, a class of drugs hitherto eschewed by kidney doctors for fear of high potassium levels. Finerenone reduces not just proteinuria, but it is accepted wisdom that, like all other mineralocorticoid receptor antagonists, it reduces fibrosis, inflammation, and oxidative stress in the body. So far, we have only two significant studies analyzing finerenone, and both of them showed improvement in protein leakage in diabetic kidney disease patients. True, current research limits the use of fineronone to only kidney patients with diabetes, but I believe its indications will soon extend beyond diabetic kidney disease.
You might be already tired of reading this tirade of kidney disease treatments, but we are only halfway through.
A Drug to Fight Obesity
On October 10, 2023, a research trial, FLOW, was stopped earlier for its efficacy results, for interim analysis met pre-specified criteria. The FLOW trial intended to study the benefits of Semaglutide (a drug more commonly known as Ozempic) in kidney disease patients with diabetes. We don’t have the final results of the study available yet, but the surprise has already gone: Novo Nordisk announced the results of the trial in a newsletter on March 5, 2024, declaring a whooping 27 percent reduction in the kidney disease-related health problems in patients with diabetes. Semaglutide is a GLP-1 agonist, a class of drugs that mimic the function of a natural hormone glucagon-like peptide-1 (GLP-1), that works at the level of our gut as well as the brain, realigning multiple hormonal axes in the body in favor of weight loss. No wonder semaglutide showed such incredible kidney disease-related results, for we now know very well the role of metabolic disturbances, including insulin resistance and obesity, in causing and worsening kidney disease. In fact, many GLP-1 agonists’ earlier research trials, between 2015 and 2022, consistently showed better kidney profiles in patients taking these drugs compared to placebo, mentally preparing us for the remarkable outcomes seen in the FLOW.

At any rate, the FDA has already approved semaglutide “to reduce the risk of cardiovascular death, heart attack, and stroke in adults with cardiovascular disease and either obesity or overweight.” You should not be surprised if this drug gets approved for CKD in diabetic patients. It is almost written on the wall.
An Unprecedented Source of Kidneys
While some scientists were working on these drugs, another group explored solutions for kidney disease along an entirely different dimension. These researchers looked not at plants or minerals or machines; they focused on pigs instead. After years of research, this team succeeded in producing a genetically modified pig, modified such that its kidneys matched the size and protein profile of a human kidney. On March 16, 2024, doctors at Massachusetts General Hospital completed the first-ever successful pig-to-human kidney transplant, and the patient was discharged a week later, alive and kicking and smiling. This achievement has opened up new and unprecedented avenues for kidney cure. First, doctors hope to see an end, or at least a shortening, of the waiting period of many dialysis patients for transplants. Next, innovation in cloning skills might enable scientists one day to clone a kidney exactly like yours, ending the era of transplant rejection medication. Lastly, cloning pigs with human-like kidneys may change the direction and potential of kidney disease research, using pigs for trials instead of humans, removing many barriers that accompany humans as research subjects, speeding up the process and turnover time of the research results.
A Disclaimer
As this blog seeks to acquaint you with new and emerging treatments for general kidney disease, I have deliberately evaded many drugs unique to specific kidney diseases: spartan and budesonide for IgA nephropathy, voclosporin and belimumab for lupus nephritis, etc.
Before concluding the essay, I would like to insert a short disclaimer. All the treatments mentioned in the blog are not a replacement for a healthy lifestyle. Inevitable as it is, a healthy lifestyle is a must, whether you have kidney disease or not, whether you are on medicines or dialysis.
What Do We Need to Do?
Simply put, we now have a myriad of treatment options for kidney disease, medicines that are not in the pipeline or decades away from us but rather available at our local drug stores. Except for gene-edited pig kidneys, all other treatment options are available worldwide and affordable for most patients. Our doctors and patients must learn about these promising treatments, their benefits, and their side effects. Our doctors, in particular, must also learn how to navigate through these drugs’ financial and clinical complexities so that none of their kidney disease patients remain behind. Remember that the complexities of these treatments are nothing compared to the ones caused by kidney disease.