Do you know what is residual renal function?
Along with other million questions in the mind of a dialysis patient, one question outweighs every other concern—”How would dialysis affect my kidneys?”
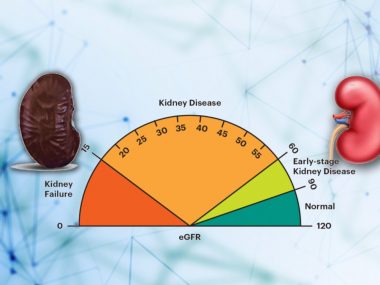
A patient is started on dialysis when he develops symptoms that cannot be relieved despite optimum therapy, and, usually, the patient’s kidney function has at this stage already declined to less than ten percent. Yet, this remaining ten percent functioning, or even less in some cases, holds great value for the well-being of the patient. In medical jargon, these last few breaths of the failing kidneys are called “residual kidney function.”
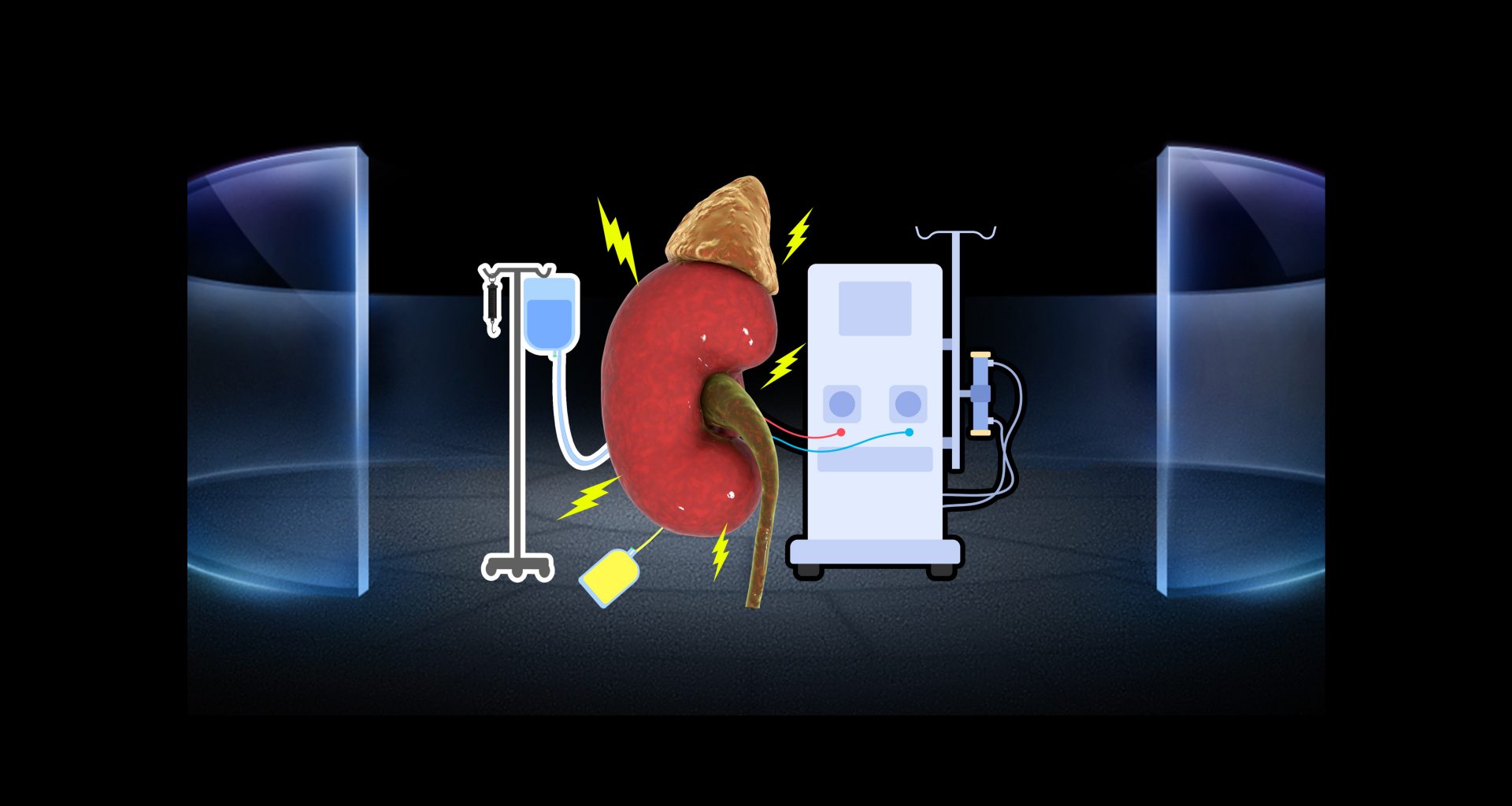
Of the two types of dialysis—hemodialysis and peritoneal—it is hemodialysis that adversely affects kidney function faster. Due to this reason, peritoneal dialysis is a preferred choice of nephrologists in developed countries (more on this in future blogs). For now, this digressive paragraph’s purpose is to emphasize that the interplay between dialysis and kidney function explained in this blog concerns hemodialysis, with the occasional mention of peritoneal dialysis only where strictly needed.
Value of Residual Renal Function in Dialysis Patient
Our kidneys are invaluable. Every bit of glomerular filtration rate contributes directly to the patient’s quality of life. Typically, we don’t measure kidney function in bits, but CKD patients can relate to this way of looking at kidney function well, for only a kidney disease patient can know the value each milliliter of glomerular filtration rate holds. In dialysis patients, this realization takes on an entirely new reality. They learn to measure and value kidney function literally in drops of urine they produce daily, every milliliter being viewed as some sacred fluid, the flow of which needs to be preserved.
Measurement of Residual Renal Function
Measuring renal function in dialysis patients comes with many challenges. Plasma concentration of urea and creatinine, our primary markers for measuring kidney function, prove useless for eGFR estimation in dialysis patients. Being largely removed during the process of dialysis, creatinine loses its consistency as a marker of kidney function.
Cystatin C, another body protein commonly used for measuring eGFR in CKD patients, has yet to be thoroughly investigated in dialysis patients. Similarly, external markers, such as Inulin and Cr-EDTA, prove labor-intense and time-consuming, making them a less likely choice for use in dialysis patients.
Currently, the only reliable and most practical method for eGFR in dialysis patients is 24-hour urine creatinine clearance, calculated by measuring 24-hour urine creatinine and urea along with random serum creatinine.
How Does Dialysis Affect Residual Renal Function
Both hemodialysis and peritoneal dialysis affect residual renal function. Hemodialysis, however, exerts a more forceful influence in a rapid fashion.
Typically, stage 5 CKD patients (pre-dialysis patients, in other words) are characteristically volume overloaded and uremic. In addition, their kidneys have an impaired ability to regulate salt and water excretion. Both these features contribute to maintaining urine volume in late-stage CKD patients. Hemodialysis significantly reverses both volume expansion and uremia, markedly reducing the urine output soon after starting the dialysis. These sudden changes in creatinine, urea, and water impair kidney function even more.
Large volume removal in hemodialysis also causes unhealthy changes in blood pressure, resulting in low blood pressure between dialysis days, called interdialytic hypotension, which directly damages the kidneys.
In addition to sudden and severe changes in blood pressure, volume, and uremia, hemodialysis carries some inherent risk factors that expose the body and kidneys to unwanted harmful elements. For example, hemodialysis uses astonishingly large quantities of water—192 liters or about 50 gallons—for one treatment. If a patient is exposed to so much water that is not ultra-purified, one can only imagine the damage. Similarly, the dialysis filter’s membrane can react when it comes in contact with the blood, releasing inflammatory chemicals from various blood cells.
How Quickly Does Residual Renal Function Decline?
Most literature on residual renal function focuses on the first year after dialysis, possibly because the most significant changes in residual renal function occur during this period. Consequently, our information regarding kidney function beyond the first year on dialysis remains sketchy. At any rate, some studies show that 14 to 20 percent of patients still have some residual renal function even three to five years after starting hemodialysis.
Patients on peritoneal dialysis enjoy their residual renal function for much longer.
What Can You Do to Preserve Residual Renal Function?
The decline in RRF is inevitable. In most cases, the primary renal disease has set in the process of progressive damage that continues even after starting dialysis, not to mention the process of dialysis itself that contributes its own damage to the kidney. The focus of management in a dialysis patient should be on mitigating the factors that are modifiable, preserving the residual function for as long as possible.
A Good Dialysis
Ideal dialysis requires teamwork. The patient, the nephrologist, and the ancillary team, including the dialysis technician, nutritionist, and social worker— all need to play their part.
Besides biocompatible membranes, the latest machines, and ultra-purified water, ideal dialysis needs patient compliance: three dialyses per week, each lasting four hours, regular medicine intake, and a religious dietary regime.
Manage Primary Renal Disease
The RRF decline progresses more rapidly in some kidney diseases compared to others. Glomerular diseases, including diabetes, for example, manifest a more rapid decrease in RRF than tubulointerstitial disease. It means treating the underlying illness is as important in dialysis patients as it is in a pre-dialysis patient. Likewise, an autoimmune disorder, such as Lupus or vasculitis, should be treated with immunosuppressives or appropriate medications.
Manage Other Illnesses
A dialysis patient must also manage other body conditions, such as diabetes, high blood pressure, and heart failure, even when they are not directly responsible for kidney disease.
Healthy Life Style
Lifestyle can make a significant difference. Do regular exercise. Clock in eight hours of sleep. Quit smoking.
Dietary Hygiene
Proteins
Guidelines recommend high protein intake in hemodialysis patients—1.2 gm per kilogram of ideal body weight. Protein intake of less than this amount has been linked with poor outcomes in these patients.
On the other hand, low protein intake, when combined with ketoanalogues, helps preserve the residual renal function in peritoneal dialysis patients.
Water and Salt
As renal function declines, water and salt regulation goes off the rails. A dialysis patient must watch what he drinks and how much salt he consumes. Overhydration means high blood pressure and work overload on your heart, whereas dehydration causes low blood pressure. Both overhydration and dehydration adversely affect residual renal function.
Healthy Diet
A healthy diet for dialysis patients includes all the typical items considered healthy for the general population—fresh fruits and vegetables, unrefined carbohydrates, and unsaturated fats—but with some limitations. Dialysis patients have to be careful with natural foods rich in phosphorus and potassium.
Medications
Blood Pressure Medicines
We still need more consensus on what blood pressure medication should primarily be used for dialysis patients. However, all doctors agree that better blood pressure control is essential for dialysis patients.
Diuretics
Diuretics like Lasix and torsemide help maintain fluid and salt balance even in dialysis patients, particularly those who continue to make more than 100 ml of urine daily. Better fluid and salt management means better blood pressure control and less stress on the kidney.
Phosphate Binders
No dialysis patient prescription is complete without a phosphate binder, for despite dietary phosphorus restriction and regular dialysis, it is hard to optimize blood phosphorus levels. High blood phosphate levels lead to hardening of blood vessels and worsening kidney function in pre-dialysis patients. In this scenario, phosphate binders prove to be a godsend.
Avoid Nephrotoxins
All pharmaceutical or plant-based products that are harmful to CKD patients can damage residual renal function in dialysis patients. Certain medications, such as ibuprofen and naproxen, top this list. Likewise, some antibiotics may directly damage the kidney, and their dose should be monitored closely.
Radiocontrast agents are also in the league of nephrotoxic compounds, and whenever a dialysis patient needs a CT scan or any other procedure that requires dye, he should involve his kidney disease doctor.
Take Home
Residual renal function is like a second lifeline for a dialysis patient, the first being dialysis itself. You should take every step to preserve your residual renal function, for better residual renal function means better quality of life.