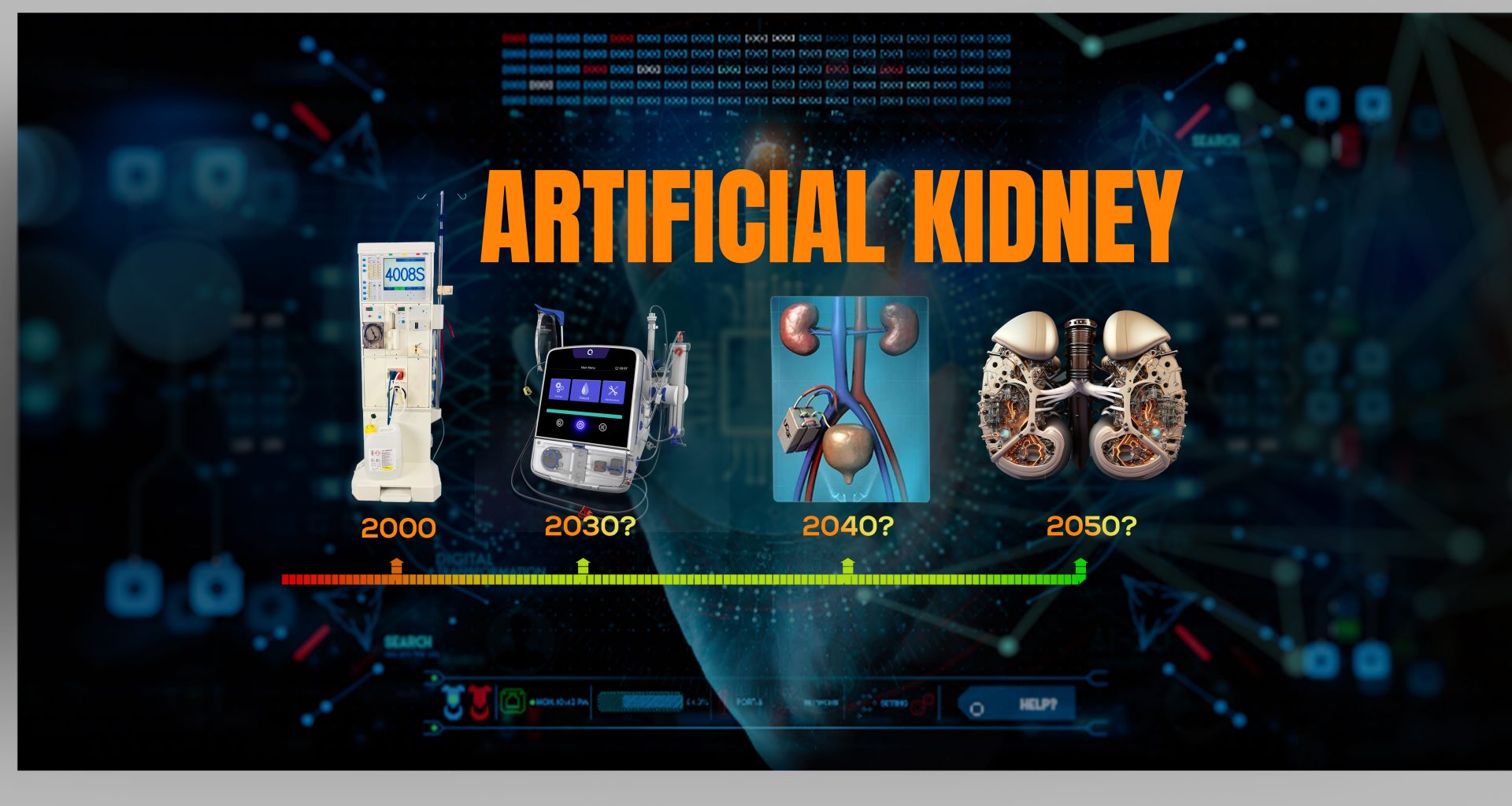
The arrival of the artificial kidney will be sooner than you think. However, this marvel will have a mixed profile: some of its features may exceed your expectations, while others might be disappointing.
An artificial kidney would be a revolutionary device that may transform the future of kidney care, but when a layperson hears about artificial kidney, his mind conjures up some fictional machine out of a Marvel movie, a device made of a super-natural element that would be safe, strong, resilient, and self-sufficient.
In reality, the artificial kidney is just an idea, and different groups are developing this idea in various forms, depending upon their resources, scientific background, and even evolutionary beliefs.
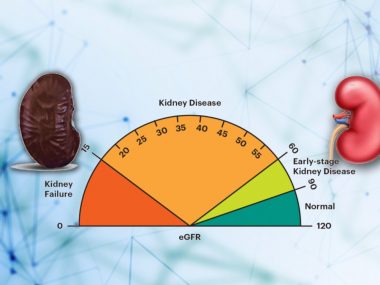
As a nephrologist, I want my patients to learn about this revolutionary device but in realistic terms. Therefore, before embarking on this journey, we must understand two basic things: First, what do we have against dialysis? Second, even if dialysis is not a perfect solution for kidney failure patients, what about kidney transplants?
Dialysis (Hemodialysis)
Dialysis is not just a life-saving treatment for end-stage renal failure patients. Since its introduction about six decades ago, this method has been the mainstay of treatment for kidney failure patients.
Yet, its technique hasn’t improved much. Despite improvements in the essential parts used in the process—Fluid, filter, pump—dialysis has barely shown better results. At the end of the first quarter of the twenty-first century, dialysis can do only two of the many kidney functions—filtration and water and electrolyte balance—that too only clumsily.

To achieve even this much, dialysis requires expensive machines, sophisticated medical set-up, highly trained professionals (medical and non-medical), and a lot of water (120 to 180 Liters of water for one dialysis ). Worst of all, it takes a toll on patients’ quality of life: traveling is almost impossible, full-time work is out of the question, and patients become utterly dependent on the State or family—patients’ lives turning into a socially limited existence.
Kidney Transplant
A kidney transplant is incredible. After the transplant, the patient comes off dialysis and many medications and restores to normal health and life, as if he has never been through the nightmare of being on dialysis. The patient has to take a few medications, called immunosuppressives, for the rest of his life, but he welcomes this slight bother with arms wide open and eyes full of tears, considering what life was like before the transplant. Kidney transplant lasts about ten to fourteen years, and one can receive another transplant once the first one fails, and then another if needed.
There is a small problem, however. We don’t have enough kidneys to transplant. Consequently, many patients die while waiting for a donor kidney.
Artificial kidney
Being a kidney disease doctor, you often feel that innovations and improvements in dialysis and transplant have reached a standstill. Neither dialysis nor transplant has seen any breakthroughs in the last decade. Consequently, scientists are shifting their focus to something else entirely—a machine that will mimic native human kidneys and is generally known as an artificial kidney.
Different groups are working day and night to come up with a meticulous machine (note that it will still be a machine, however sophisticated it may be) that would take the filtration function of dialysis as close to the native kidney as possible without needing a gigantic apparatus and dozens of gallons of water. So far, three prototypes are on the horizon.
Portable Devices
A portable device weighing around ten kilos and working without requiring external water connections sounds more practical than a wearable or implantable dialysis machine. This is the model of the artificial kidney that we would see in the market in the coming years.
One such device is underway in Seattle, USA, where a scientist and a bioengineer are working together to develop a machine that would be able to recycle dialysate—the fluid that removes urea and adds back electrolytes. The magic machine is equipped with a regeneration module. Once dialysate picks up urea from the blood, it passes through this module, where ultraviolet light splits the absorbed urea into nitrogen and carbon dioxide that vaporizes into the air, and the purified dialysate flows back to pick up more urea. This mechanism allows the machine to perform dialysis without using liters of water to flush out nitrogenous waste products, the first step toward portability. Another welcome feature is its size: weighing only fourteen kilograms or less, the device is portable as well as travel-friendly.

Similarly, US Kidney Research Corporation in Roseville, California, is working on another suitcase-sized device that is expected to replicate the filtration function of our biological kidney without relying on living cells. To achieve this incredible feat, the machine relies on an ultrafiltration module that contains a cellulose-based membrane, able to filter more volume per surface area compared to the existing polythene membranes used in hemodialysis. Only water, urea, and electrolytes pass this filter, while blood cells and proteins cannot. The filtrate—fluid containing water, urea, and electrolytes—then passes through a nanofiller with even smaller pores, small enough to block the movement of the glucose molecule, which also stays in the blood. Next come deionization modules, basically a superb use of an old technique in which electrical charges control the movement of ions such as sodium, potassium, calcium, and phosphorus, removing only as much as is required and returning the remaining amount into the blood. Finally, this synthetic urine passes through an osmosis module that transports the water back to the blood.
In addition to their benefits of portability and emancipation from a serious water supply, these machines would allow slow, constant dialysis, avoiding major swings in the volume, urea, and electrolytes, a common characteristic mainly of in-center hemodialysis and associated with poor health outcomes.
Bioartificial Kidney
The organoid I am going to describe in this section might match the artificial kidney of your imagination. It all started in 2004 when researchers connected the traditional dialysis cartridge to another module lined with human kidney cells. The idea was to be able to reclaim water and electrolytes, such as sodium and potassium, with minimal to no cytokine production. The project was initially intended for traumatic acute kidney injury patients and reached the stage of clinical trials.
However, the idea was later taken up by the Kidney Project, a research program run by the University of California, San Francisco, and has now turned into a national research program where scientists hope to develop a bioartificial kidney that would be wearable— and ultimately implantable.
How do they plan to produce such a fictional device? In our logical world, where we expect and opt for linear evolution of things, the Kidney Project team is taking a non-traditional approach, harnessing the technological achievements of various fields to produce a device that will be a machine but behave like an organ.
The bioartificial kidney consists of two parts.
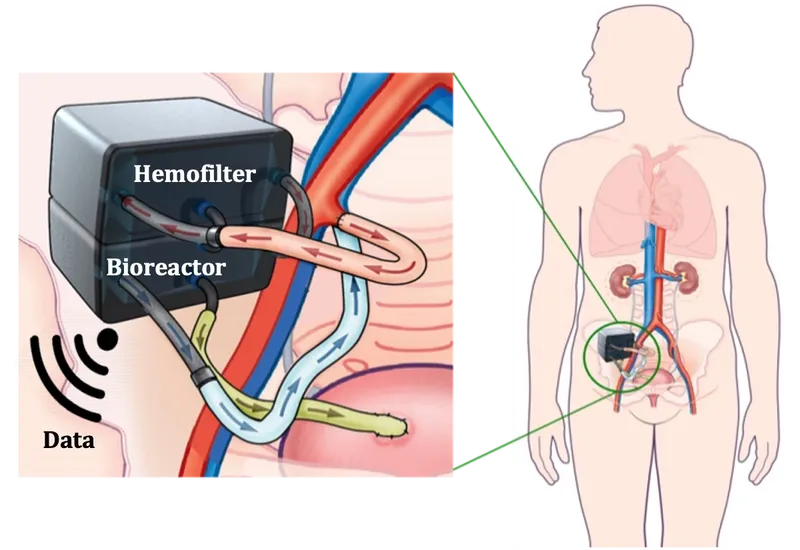
Filter
The filter is not a foot-long cylinder filled with polythene membrane; instead, the filter consists of a silicon chip, a chip similar to the one used in computers and cell phones, with three unique characteristics. This chip filter is so thin that the body’s own blood pressure is enough to drive blood through it, excluding the need for a pump. Then, slits on the chip are more uniform, giving the filter better selectivity, allowing only specific molecules, such as urea, to get through while retaining bigger objects, such as blood cells. Furthermore, the chip has a coating of a material, such as polyethylene glycol, that prevents protein accumulation, preventing blood clots.
Bioreactor
If your jaw dropped from learning about silicon chips as a filter, it might blow your mind that Kidney X team is working on a reactor lined with kidney cells. Living-cells-lined reactor mimics the function of a kidney tubule, transporting essential electrolytes like sodium and potassium back into the blood and draining excess water and toxins into the bladder. Since we now have original kidney cells involved in this process, wouldn’t the body mount a reaction against these foreign intruders? The answer is “No.” You saw that slits in the silicon chip are too small to allow immune cells to pass through, which means these cells would never reach the reactor, allowing us to use the device without fearing an immune reaction. One can also infer, then, that patients won’t have to use immunosuppressive medications, giving bioartificial kidneys an advantage over living kidney transplants.
Imperfections of the Artificial Kidney
Still, despite its apparent promise, the bioartificial kidney carries some inherent imperfections that must need consideration. First is the limited lifespan of the device, which is rumored to be around five years. It means that if this bioartificial kidney works as we expect, and improves the quality of life, helping patients live a longer life, the patient had to exchange the device every five years or so. The second easily foreseeable issue surrounding its availability, particularly in the developing countries, would be its prohibitive cost.
Would Artificial Kidney be the End of Dialysis and Transplant
Even though artificial kidney appears to be a promising treatment for end-stage-renal-disease patients, it would be absurd to say that this new technology would push hemodialysis and transplants into oblivion. Even after its realization into the most practical form, the device would not be as readily and widely available as many of us would like to believe. Furthermore, dialysis and transplant would have seen some improvements by then, making them a cheaper and more accessible option for most kidney disease patients across the globe. In short, I don’t see the artificial kidney replacing dialysis and transplant in the coming decades.
Take Home
Artificial kidney clearly manifests the human potential for innovation. Many scientists are working day in and day out on these projects to improve kidney disease patients’ lives.
However, we may be many years away from a commercially available artificial kidney. I expect the portable version to be available within a decade, while the wearable or implantable kidney might take a little longer. Until then, we better make the most of what we have: Kidney disease patients must nurse every bit of their kidney function; dialysis patients work diligently with their dialysis team; and all of us help promote the culture of a kidney transplant.